Publications
Waigi, et al.
GeroScience — June 2024
-
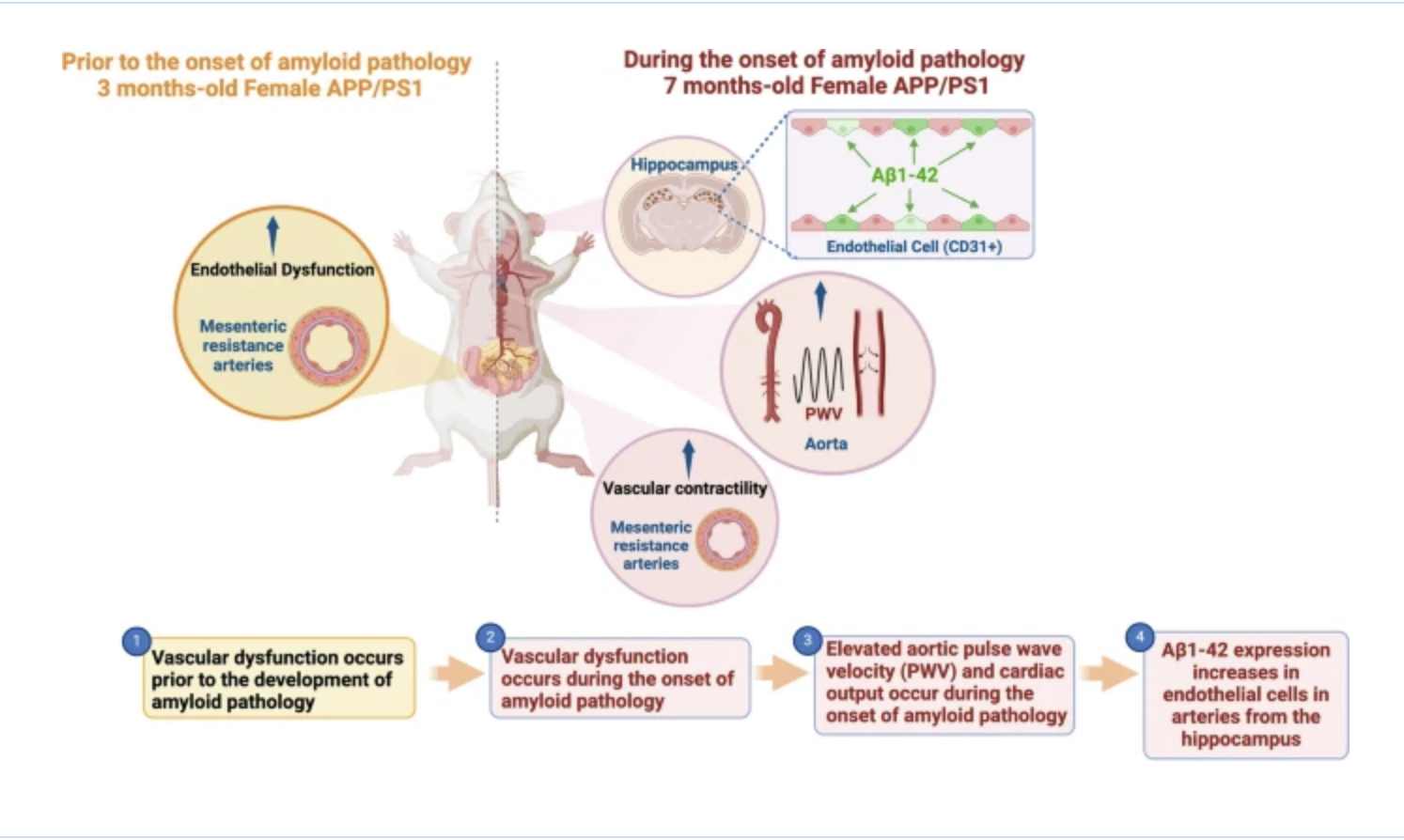
Increasing evidence shows that cardiovascular diseases (CVDs) are associated with an increased risk of cognitive impairment and Alzheimer’s diseases (AD). It is unknown whether systemic vascular dysfunction occurs prior to the development of AD, if this occurs in a sex-dependent manner, and whether endothelial cells play a role in the deposition of amyloid beta (Aβ) peptides. We hypothesized that vascular dysfunction occurs prior to the onset of amyloid pathology, thus escalating its progression. Furthermore, endothelial cells from female mice will present with an exacerbated formation of Aβ peptides due to an exacerbated pressure pulsatility. To test this hypothesis, we used a double transgenic mouse model of early-onset AD (APPswe/PSEN1dE9). We evaluated hippocampus-dependent recognition memory and the cardiovascular function by echocardiography and direct measurements of blood pressure through carotid artery catheterization. Vascular function was evaluated in resistance arteries, morphometric parameters in the aortas, and immunofluorescence in the hippocampus and aortas. We observed that endothelial dysfunction occurred prior to the onset of amyloid pathology irrespective of sex. However, during the onset of amyloid pathology, only female APP/PS1 mice had vascular stiffness in the aorta. There was elevated Aβ deposition which colocalized with endothelial cells in the hippocampus from female APP/PS1 mice. Overall, these data showed that vascular abnormalities may be an early marker, and potential mediator of AD, but exacerbated aortic stiffness and pressure pulsatility after the onset of amyloid pathology may be associated with a greater burden of Aβ formation in hippocampal endothelial cells from female but not male APP/PS1 mice.
Pernomian, et al.
Preprint — May 2024
-
Background: Small artery remodeling and endothelial dysfunction are hallmarks of hypertension. Growing evidence supports a likely causal association between cardiovascular diseases and the presence of endothelial-to-mesenchymal transition (EndMT), a cellular transdifferentiation process in which endothelial cells (ECs) partially lose their identity and acquire additional mesenchymal phenotypes. EC reprogramming represents an innovative strategy in regenerative medicine to prevent deleterious effects induced by cardiovascular diseases.
Methods: Using a partial reprogramming of ECs, via overexpression of Oct-3/4, Sox-2, and Klf-4 (OSK) transcription factors, we aimed to bring ECs back to a youthful phenotype in hypertensive mice. Primary ECs were infected with lentiviral vectors (LV) containing the specific EC marker cadherin 5 (Cdh5) and the fluorescent reporter enhanced green fluorescence protein (EGFP) with empty vector (LVCO) or with OSK (LV-OSK). Confocal microscopy and western blotting analysis were used to confirm the OSK overexpression. Cellular migration, senescence, and apoptosis were evaluated. Human aortic ECs (HAoECs) from male and female normotensive and hypertensive patients were analyzed after OSK or control treatments for their endothelial nitric oxide synthase (eNOS) levels, nitric oxide (NO), and genetic profile. Male and female normotensive (BPN/3J) and hypertensive (BPH/2J) mice were treated with an intravenous (i.v.) injection of LVCO or LV-OSK and evaluated 10 days post-infection. The blood pressure, cardiac function, vascular reactivity of small arteries, in vivo EGFP signal and EndMT inhibition were analyzed.
Results: OSK overexpression induced partial EC reprogramming in vitro , and these cells showed endothelial progenitor cell (EPC)-like features with lower migratory capability. OSK treatment of hypertensive BPH/2J mice normalized blood pressure and resistance arteries hypercontractility, via the attenuation of EndMT and elastin breaks. EGFP signal was detected in vivo in the prefrontal cortex of both BPN/3J and BPH/2J-treated mice, but OSK induced angiogenesis only in male BPN/3J mice. OSK-treated human ECs from hypertensive patients showed high eNOS activation and NO production, with low ROS formation. Single-cell RNA analysis showed that OSK alleviated EC senescence and EndMT, restoring their phenotypes in human ECs from hypertensive patients.
Conclusion: Overall, these data indicate that OSK treatment and EC reprogramming can decrease blood pressure and reverse hypertension-induced vascular damage
Wenceslau, et al.
Hypertension — February 2024
-
To celebrate 100 years of AHA-supported cardiovascular disease research, this review article highlights milestone papers that have significantly contributed to the current understanding of the signaling mechanisms driving hypertension and associated cardiovascular disorders. This article also includes a few of the future research directions arising from these critical findings. To accomplish this important mission, 4 principal investigators gathered their efforts to cover distinct yet intricately related areas of signaling mechanisms pertaining to the pathogenesis of hypertension. The renin-angiotensin system, canonical and novel contractile and vasodilatory pathways in the resistance vasculature, vascular smooth muscle regulation by membrane channels, and noncanonical regulation of blood pressure and vascular function will be described and discussed as major subjects.
Bernardino de Paula, et al.
Heart And Circulatory Physiology — November 2023
-
Aging is associated with cognitive decline via incompletely understood mechanisms. As individuals grow older, the processes regulating cerebral blood flow and vascular function in the brain microcirculation may become compromised and elevate the risk of neurodegenerative conditions. Small focal hypoxic and ischemic events in the brain can potentially coalesce into more significant lesions, ultimately exacerbating cognitive decline and the risk of developing dementia (1).
Intracerebral parenchymal arterioles (PAs) dive deep into the brain parenchyma and play a critical role in maintaining the appropriate perfusion pressure via myogenic tone and/or autoregulation in the brain microcirculation, safeguarding capillaries from the harmful effects of elevated intravascular pressure. These arterioles are high-resistance blood vessels with internal diameters ranging from 20 to 70 μm, and they represent the most distal arteries that contain vascular smooth muscle cells (VSMCs). Unlike the brain’s surface pial arteries, PAs lack collateral branches and anastomoses, making them indispensable “bottlenecks” in the cerebral circulation (2).
Costa, et al.
Clinical Science — November 2023
-
DescriptO-Linked attachment of β-N-acetylglucosamine (O-GlcNAc) on serine and threonine residues of nuclear, cytoplasmic, and mitochondrial proteins is a highly dynamic and ubiquitous post-translational modification that impacts the function, activity, subcellular localization, and stability of target proteins. Physiologically, acute O-GlcNAcylation serves primarily to modulate cellular signaling and transcription regulatory pathways in response to nutrients and stress. To date, thousands of proteins have been revealed to be O-GlcNAcylated and this number continues to grow as the technology for the detection of O-GlcNAc improves. The attachment of a single O-GlcNAc is catalyzed by the enzyme O-GlcNAc transferase (OGT), and their removal is catalyzed by O-GlcNAcase (OGA). O-GlcNAcylation is regulated by the metabolism of glucose via the hexosamine biosynthesis pathway, and the metabolic abnormalities associated with pathophysiological conditions are all associated with increased flux through this pathway and elevate O-GlcNAc levels. While chronic O-GlcNAcylation is well associated with cardiovascular dysfunction, only until recently, and with genetically modified animals, has O-GlcNAcylation as a contributing mechanism of cardiovascular disease emerged. This review will address and critically evaluate the current literature on the role of O-GlcNAcylation in vascular physiology, with a view that this pathway can offer novel targets for the treatment and prevention of cardiovascular diseases.ion text goes here
Costa, et al.
Hypertension — November 2022
-
Hypertension is the most important risk factor for the development of terminal cardiovascular diseases, such as heart failure, chronic kidney disease, and atherosclerosis. Lifestyle interventions to lower blood pressure are generally desirable prior to initiating pharmaceutical drug treatments, which may have undesirable side effects. Ketogenic interventions are popular but the scientific literature supporting their efficacy is specific to certain interventions and outcomes in animal models and patient populations. For example, although caloric restriction has its own inherent difficulties (e.g. it requires high levels of motivation and adherence is difficult), it has unequivocally been associated with lowering blood pressure in hypertensive patients. On the other hand, the antihypertensive efficacy of ketogenic diets is inconclusive, and this is surprising, given that these diets have been largely helpful in mitigating metabolic syndrome and promoting longevity. It is possible that side effects associated with ketogenic diets (e.g. dyslipidemia) aggravate the hypertensive phenotype. However, given the recent data from our group, and others, reporting that the most abundant ketone body, β-hydroxybutyrate, can have positive effects on endothelial and vascular health, there is hope that ketone bodies can be harnessed as a therapeutic strategy to combat hypertension. Therefore, we conclude this review with a summary of the type and efficacy of ketone supplements. We propose that ketone supplements warrant investigation as low-dose antihypertensive therapy that decreases total peripheral resistance with minimal adverse side effects.